The scaphoid bone is one of the eight small bones that comprise the
wrist joint. The two rows of small wrist bones act together to allow the
wide variety of wrist positions and motions that we take for granted.
The scaphoid bone spans or links these two rows together and, therefore
has a special role in wrist stability and coordinating wrist motion (see
Figure 1).
The scaphoid bone is vulnerable to fracture because of its position
within the wrist and its role in wrist function. When the scaphoid bone
is broken, it may not heal properly because it has a very fragile blood
supply. Scaphoid fractures that do not heal are referred to as a
scaphoid non-union. Ultimately, scaphoid non-unions can lead to loss of
wrist motion and eventual wrist arthritis.
Patients with a scaphoid non-union usually present with a history of
previous wrist injury, especially a fall onto an outstretched wrist.
They will typically have pain along the thumb side of the wrist and may
also have diminished wrist mobility, particularly wrist extension.
Scaphoid fractures and non-unions are usually confirmed by x-rays of the
wrist (see Figure 2A and 2B). In many cases, special x-ray tests are
also used to decide the best treatment approach. A CT scan is helpful to
check for collapse of the scaphoid on itself, resulting in a bend in the
bone, which is called a “humpback” deformity (see Figure
3).
Scaphoid non-unions may also develop a problem called avascular
necrosis. Avascular necrosis occurs when part of the scaphoid bone dies
because of the loss of blood flow. This can eventually result in
fragmentation and the collapse of the bone. Its presence also makes
repair of the scaphoid much more difficult. An MRI scan can be helpful
to check for avascular necrosis (see Figure 4).
Treatment of a scaphoid non-union is dependent upon a variety of
factors. Once a scaphoid fracture has failed to heal, a relatively
predictable pattern of degeneration within the wrist generally occurs,
although the time frame is variable. In most cases, the scaphoid
eventually collapses, which results in a change in wrist mechanics that
leads to motion loss and arthritis. Depending upon the stage of this
process at which the non-union is recognized, various treatment
alternatives exist. In cases without significant arthritis, surgery to
restore scaphoid alignment and heal the bone is preferred. This usually
requires placement of a bone graft and some type of internal bone
fixation, such as pins or a screw (see Figure 5).
Scaphoid non-unions with avascular necrosis present special challenges
to healing since part of the bone is dead. Recent techniques using bone
grafts with an attached vessel to maintain blood supply (vascularized
bone grafts) have improved our ability to heal these difficult
conditions (see Figure 6).
Finally, in cases with established arthritis or failed reconstructive
efforts, surgery to heal the scaphoid is often no longer an option. In
these cases, surgery is tailored towards pain improvement along with
maintaining a functional wrist. Depending on the degree of arthritis,
surgery may include techniques that spare motion, such as radial
styloidectomy (removal of a local piece of arthritic bone), partial
fusion of the wrist bones, or proximal row carpectomy (removal of the
proximal row of wrist bones). If the arthritis is more widespread in the
wrist, complete wrist fusion may be needed.
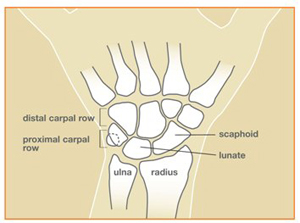
Figure 1: Wrist bone anatomy

Figure 2A: X-ray of scaphoid fracture non-union

Figure 2B: X-ray of normal scaphoid
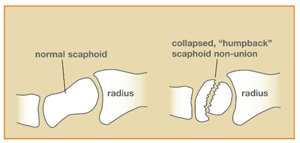
Figure 3: Diagram of normal and collapsed scaphoid

Figure 4: MRI of scaphoid fracture non-union with avascular
proximal fragment

Figure 5: Scaphoid repaired with a screw

Figure 6: Vascularized bone graft for scaphoid
© 2006 American Society for Surgery of the Hand





