What is tennis elbow/lateral epicondylitis?
Lateral epicondylitis, commonly known as tennis elbow, is a painful condition involving the tendons that attach to the bone on the outside (lateral) part of the elbow. Tendons anchor the muscle to bone. The muscle involved in this condition, the extensor carpi radialis brevis, helps to extend and stabilize the wrist (see Figure 1). With lateral epicondylitis, there is degeneration of the tendon's attachment, weakening the anchor site and placing greater stress on the area. This can then lead to pain associated with activities in which this muscle is active, such as lifting, gripping, and/or grasping. Sports such as tennis are commonly associated with this, but the problem can occur with many different types of activities, athletic and otherwise.
What causes tennis elbow/lateral epicondylitis?
Who gets tennis elbow/lateral epicondylitis?
The most common age group that this condition affects is between 30 to 50 years old, but it may occur in younger and older age groups, and in both men and women.
Signs and symptoms of tennis elbow/lateral epicondylitis
Pain is the primary reason for patients to seek medical evaluation. The pain is located over the outside aspect of the elbow, over the bone region known as the lateral epicondyle. This area becomes tender to touch. Pain is also produced by any activity which places stress on the tendon, such as gripping or lifting. With activity, the pain usually starts at the elbow and may travel down the forearm to the hand. Occasionally, any motion of the elbow can be painful.
Treatment for tennis elbow/lateral epicondylitis
Conservative (non-surgical)
Activity modification - Initially, the activity causing the condition should be limited. Limiting the aggravating activity, not total rest, is recommended. Modifying grips or techniques, such as use of a different size racket and/or use of 2-handed backhands in tennis, may relieve the problem.
Medication - anti-inflammatory medications may help alleviate the pain.
Brace - a tennis elbow brace, a band worn over the muscle of the forearm, just below the elbow, can reduce the tension on the tendon and allow it to heal.
Physical Therapy - may be helpful, providing stretching and/or strengthening exercises. Modalities such as ultrasound or heat treatments may be helpful.
Steroid injections - A steroid is a strong anti-inflammatory medication that can be injected into the area. No more than (3) injections should be given.
Shockwave treatment - A new type of treatment, available in the office setting, has shown some success in 50 - 60% of patients. This is a shock wave delivered to the affected area around the elbow, which can be used as a last resort prior to the consideration of surgery.
Treatment is designed to relieve pain and restore function. If you have rheumatoid arthritis in your hands, medications can help decrease inflammation, relieve pain and slow the progression of the disease. Anti-inflammatory medications, oral steroids, and/or cortisone injections may be used. Several disease-modifying treatments are now available, including anti-malarial drugs, methotrexate, cyclosporine, gold, and other new drugs (remicade, enbrel) that help suppress the body's immune system to reduce the inflammation and pain. A rheumatologist will often prescribe and monitor these types of medications. Your physician may also refer you to a hand therapist for exercises, splints, modalities such as paraffin (warm wax) baths, and instruction on how to use your hands in ways that may help relieve pain and pressure and also protect your joints. Adaptive devices may help you cope with the activities of daily living.
Rheumatoid arthritis often affects the tendons as well as the joints. The tendons that become inflamed may trigger (click) or rupture. If this happens, you may be unable to bend or straighten your fingers or to grip properly. In certain cases, specific preventive surgery may be recommended. Preventive surgery may include removing nodules, releasing pressure on tendons by removing the inflamed tissue and degenerated, rough bone that may scrape the tendons, and reinforcing the tendons. If a tendon rupture has occurred, a hand surgeon may be able to repair it with a tendon transfer or graft, in addition to performing these other procedures.
Surgery to treat the arthritic joints includes removal of inflamed joint linings, joint replacements, joint fusions, and in some cases, removal of damaged bone. The specific procedure(s) depends on a variety of factors, including the particular joint(s) involved, the degree of damage present, the condition of adjacent joints, and your own needs. Your hand surgeon can help you decide on the most appropriate treatment for you.
Unfortunately, there is no cure for rheumatoid arthritis. However, surgical procedures can often help correct deformities, relieve pain, and improve function. Optimal care entails a team approach between the rheumatologist, hand surgeon, hand therapist, and patient. It is particularly important that surgical intervention be appropriately timed to rebalance the hand and preserve the joints for as long as possible, before the development of more severe deformities has occurred.
Surgery
Surgery is only considered when the pain is incapacitating and has not responded to conservative care, and symptoms have lasted more than six months. Surgery involves removing the diseased, degenerated tendon tissue. Two surgical approaches are available; traditional open surgery (incision), and arthroscopy — a procedure performed with instruments inserted into the joint through small incisions. Both options are performed in the outpatient setting.
Recovery
Recovery from surgery includes physical therapy to regain motion of the arm. A strengthening program will be necessary in order to return to prior activities. Recovery can be expected to take 4-6 months.
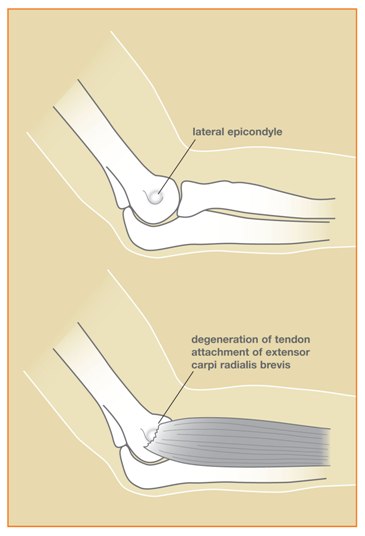
Figure 1: The muscle involved in this condition, the extensor carpi radialis brevis, helps to extend and stabilize the wrist